Over fifty percent of the global population is affected by headache disorders every year, with fourteen percent suffering from migraines. That’s a lot of pain that half the world regularly faces — and the easiest way many of us manage this pain is through a quick trip to the drugstore for a bottle of Aspirin. While pain-relief medications may be easy and effective, long-term use of these medications can negatively affect your body, likely resulting in even more headaches and migraines.
Natural Headache Relief 101
If you suffer from chronic pain or headaches, chances are you’ve relied on the fast-acting effects of painkillers as the primary treatment of your pain. But your chronic use of pain-relief medication — defined as more than three times a week for more than three months — is putting you at risk for serious health issues.
However, studies show that using pain-relief medication alongside more natural alternatives is the most effective way to mitigate pain and reduce the frequency of your headaches. Your best bet at pain relief is using both alternative treatments and painkillers in moderation; this greatly reduces your risk of negative health effects over time!
Firstly, the two most essential steps in managing headaches are determining what type of headache you’re having and what could be causing your headache. There are different treatments depending on both the headache type and the potential cause of your pain.
But before attempting any new drug or treatment, or if you believe there to be serious underlying causes for your pain, make sure to consult with a doctor to do what’s best for your body.
What Kind of Headache Am I Having?
Not all pain is created equal! It’s important to determine what type of headache you’re having so you can find the most effective relief. Primary headaches are defines as head pain without any underlying diseases or problems, and there are three primary headache types:
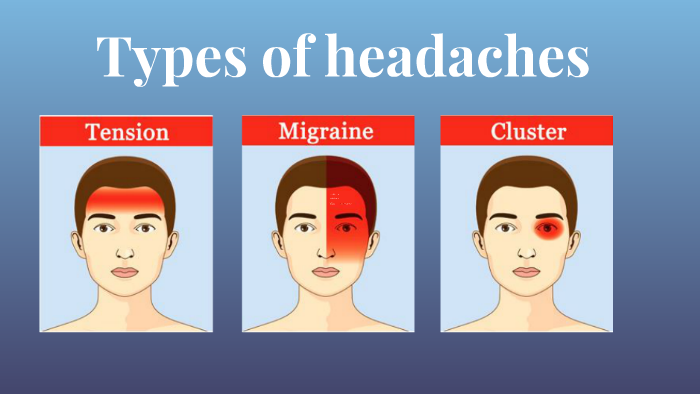
- Tension Headache: Dull, aching head pain — often described as feeling like a tight band around the head. Tension headaches can be broken down into two categories, episodic and chronic. Episodic tension headaches occur infrequently, whereas chronic tension headaches describe when your headache-having days outnumber your headache-free days.
- Migraine Headache: Severe throbbing or pulsing head pain, usually concentrated to one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last from hours to days at a time. Some migraines will be preceded by an aura — a warning symptom that can include visual disturbances such as flashes of light, or other disturbances such as difficulty speaking or tingling on one side of the face.
- Cluster Headache: Intense, piercing pain in or around one eye on one side of your head. The pain may radiate to other areas of your head, face, and neck. This type of headache strikes quickly, though you may have a migraine-like aura beforehand. Cluster headaches often occur in cluster periods — cyclical patterns — that can last from weeks to months, usually followed by a remission period where the headaches stop.
Secondary headaches are caused by underlying medical conditions such as hypertension, head injury, sinusitis, dehydration, infection, and many more. Talk to your doctor to ensure that no medical conditions or injuries could be causing your headaches.
Common Causes of Headaches and Migraines
I started dealing with chronic headaches and migraines at a young age, and for years I assumed that all my headaches — no matter what area the pain was centered in — could be treated with a few ibuprofen. While the medication helped reduce some pain, why did my headaches keep coming back?
It wasn’t until I visited a chiropractic practice to address chronic pain in my neck and shoulders that I discovered an important source of both my migraines and tension headaches: I had stiff, inflamed upper trap muscles from chronic stress! Determining the cause of your pain, especially chronic headaches and migraines, is essential for seeking out the correct treatment.
Primary headache causes include:
- Lack of sleep or poor sleep quality
- High caffeine intake or caffeine withdrawal
- Muscle tension and inflammation, especially prolonged tension
- Undereating or missing a meal
- Emotional or physical stress, often prolonged
Secondary headache causes include:
- Dehydration or related conditions that can also impair concentration and cause irritability, worsening your symptoms. Studies show that drinking more water (and increasing electrolyte consumption) reduces headache occurrence, duration, and severity in some people.
- Sleep apnea or other underlying sleep disorders
- Insulin resistance, prevalent in conditions such as PCOS and diabetes
- Medication overuse, also known as rebound headaches — approximately one to two out of every 100 people experienced rebound headaches in the past year, and they are common for people with preexisting chronic conditions. Prolonged use of over-the-counter pain relief such as acetaminophen, ibuprofen, naproxen, and combination medications such as Excedrin increases your risk of rebound headaches.
- Nutrient deficiency, such as a B12 deficiency and magnesium deficiency
- TMJ (Temporomandibular joint dysfunction)
- Gastrointestinal issues and disorders, such as GERD, IBS, Crohn’s or ulcerative colitis, Celiac disease, H. pylori infection, and GI motility disorders
- Genetics. People with a family health history of headaches, especially migraines and cluster headaches, are more prone to headache disorders
Long-term use of painkillers to treat headache disorders can exacerbate these issues — both primary and secondary — in turn making your headaches worse.
Long-term Effects of Pain Relief Medication

Three central medications used to manage headaches include Acetaminophen, NSAIDs (Nonsteroidal Anti-Inflammatory Drugs), and combination painkillers. However, when you use these painkillers as your primary treatment for recurring headaches, you open yourself up to the risk of facing a variety of nasty side effects depending on the medication — talk about my long-term use of Excedrin and my current gut issues.
Acetaminophen:
- Has a well-established history of causing both long-term liver and kidney damage and failure — acetaminophen poisoning is also responsible for nearly 50% of all acute liver failure in the US.
- Commonly reported adverse GI reactions include nausea, bleeding in the digestive tract, vomiting, and constipation.
- It also has been linked to an increased risk of heart attack, stroke, and high blood pressure.
- Acetaminophen overuse will also cause rebound headaches.
NSAIDs Such as Ibuprofen, Naproxen Sodium, and Aspirin:
- Non-aspirin NSAIDs increase the risk for heart attack, stroke, and blood clots, especially if you have preexisting heart disease or risk factors (such as smoking, high blood pressure, high cholesterol, or diabetes).
- They may increase the chance of serious GI issues like stomach ulcers, stomach irritation, and GI bleeding — this risk may be greater in people who are older, have previous history of ulcers/bleeding, are on blood thinners, drink more than three alcoholic beverages a day, or take multiple NSAID products.
- More common side effects of non-aspirin NSAIDs include increased potential for bruising, worsened asthma symptoms, and kidney damage.
- In terms of Aspirin use, studies have shown that daily aspirin use for 5-10 years can cause approximately a 7-9% decrease in cancers, but there is still proven risk of bleeding in the intestinal tract. Continued aspirin use increases the risk of peptic ulcers by 30-60%.
- NSAID overuse will also cause rebound headaches! Make sure to only take the suggested dosage.
- It should be noted that you SHOULD NOT give aspirin to a child under 18 years old to treat symptoms of fever or viral illness, as this can significantly increase their risk of developing Reye’s Syndrome.
Combination painkillers that contain several medications (such as Excedrin, Advil, Aleve, Tylenol, etc.) are the most likely to cause rebound headaches — as well as combination medications that contain Butalbital Compound such as Fiorinal, which has been shown to increase the risk of a person’s migraine progressing from episodic to chronic.
Start Soothing Your Headaches Without the Pills!

Pain relief doesn’t always have to come in pill form! You can reduce your risk of long-term health issues by using alternative treatments, lifestyle changes, and mindfulness of habits in combination with the occasional painkiller. Never settle on treating the symptom, either — talk to your doctor if you have any concerns that your headaches (episodic or chronic) could be caused by an underlying condition.
Alternative treatments for headache pain relief
- Consider manual treatments such as acupuncture, physical therapy, muscle massage, Osteopathic Manipulative Treatment, and Chiropractic therapy. I recently started going to a chiropractor for back and muscle pain, only to find out during my consultation that many of my chronic migraines are triggered by severe tightness of my suboccipital muscles. Manual treatments can provide significant pain relief!
- Acupressure has been proven to significantly improve headache symptoms. There are several pressure points on the body that will soothe headache pain!
- Try natural CGRP-inhibitors. CGRP is a protein released around the brain that dilates blood vessels and can lead to severe inflammation. In fact, it’s known as the key factor of migraine pain. Some plants can work to slow the activation of the protein — such as grape pomace — while some work at the level of the receptor sites, but sangre de drago, a supplement-like tree sap, does both by inhibiting the pain sensation and blocking inflammation response.
- Nutraceutical treatment, such as the use of magnesium (your best bet is magnesium chloride), riboflavin (vitamin B2), CoEzyme Q10, vitamin D, feverfew, and alpha-lipoic acid. Consult with your doctor before starting any new supplements!
- Melatonin supplementation will not only improve your circadian rhythm regulation and improve your quality of sleep, but they also act as an antioxidant and have pain-relieving properties. Studies show that 3 mg can be effective in adults with migraines, while 10 mg can be effective in adults with cluster headaches.
- Yoga and meditation have been proven to be effective in pain management, as well as reducing stress and enhancing your quality of life. Check out these yoga poses and the many meditations we have on the site to get started!
- To tackle primary headache causes, work on being mindful of habits that could be causing headaches. Be mindful of your diet and opt for nutrient-rich foods, ensure that you get at least eight hours of sleep, monitor your caffeine intake, and most importantly avoid prolonged stress! I know, it’s easier said than done, but studies show that stress is the most commonly reported trigger of episodic and chronic tension-type headaches.
Living with headaches, or any kind of chronic pain, is not fun. But fortunately, your pain doesn’t have to be permanent, and your headaches don’t have to limit you forever. With the right combination of integrative treatments and occasional medication use, your ability to take control of your pain will significantly improve. Next time a headache strikes and you find yourself reaching for your Aspirin, look up some acupressure points instead!
Sources
Zhou, Yingjun, et al. “Trends in the Use of Aspirin and Nonsteroidal Anti-Inflammatory Drugs in the General U.S. Population.” Pharmacoepidemiology and Drug Safety, vol. 23, no. 1, Wiley, May 2013, pp. 43–50. Crossref, doi:10.1002/pds.3463.
Over 50% of Global Population Suffer from Headache Disorders. Open Access Government, 12 Apr. 2022, https://www.openaccessgovernment.org/over-50-of-global-population-suffer-from-headache-disorders/133642/.
Gul, Fiza. Primary Headache versus Secondary Headaches. NeuroX, 25 May 2021, https://neurox.us/primary-versus-secondary-headaches/.
Tension Headache – Symptoms and Causes. Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/tension-headache/symptoms-causes/syc-20353977. Accessed 13 Oct. 2022.
Migraine – Symptoms and Causes. Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed 13 Oct. 2022.
Cluster Headache – Symptoms and Causes. Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/cluster-headache/symptoms-causes/syc-20352080. Accessed 13 Oct. 2022.
Coni, Robert. A Review of Medical Conditions That Can Cause Secondary Headaches. Med Mastery, https://www.medmastery.com/guides/headaches-clinical-guide/review-other-medical-conditions-can-cause-headache. Accessed 13 Oct. 2022.
Khorsha, Faezeh, et al. “Association of Drinking Water and Migraine Headache Severity.” Journal of Clinical Neuroscience, vol. 77, Elsevier BV, July 2020, pp. 81–84. Crossref, doi:10.1016/j.jocn.2020.05.034.
Ankar A, Kumar A. Vitamin B12 Deficiency. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441923/
Seladi-Schulman, Jill. Gastric Headache: Symptoms, Research, and More. Healthline, 26 Jan. 2021, https://www.healthline.com/health/gastric-headache#:~:text=Furthermore%2C%20a%202016%20review%20noted%20that%20over%20the,ulcers%206%20GI%20motility%20disorders%2C%20such%20as%20gastroparesis.
Van Den Maagdenberg AM, Terwindt GM, Haan J, Frants RR, Ferrari MD. Genetics of headaches. Handb Clin Neurol. 2010;97:85-97. doi: 10.1016/S0072-9752(10)97006-1. PMID: 20816412.
Lee WM. Acetaminophen and the U.S. Acute Liver Failure Study Group: lowering the risks of hepatic failure. Hepatology. 2004 Jul;40(1):6-9. doi: 10.1002/hep.20293. PMID: 15239078.
French, Aironius. The Long-Term Effects of Tylenol PM. Healthfully, 5 Dec. 2018, https://healthfully.com/the-long-term-effects-of-tylenol-pm-4423383.html.
Ashina, Sait. Stopping the Vicious Cycle of Rebound Headaches. Harvard Health, 7 Nov. 2019, https://www.health.harvard.edu/blog/stopping-the-vicious-cycle-of-rebound-headaches-2019110718180.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Cleveland Clinic, https://my.clevelandclinic.org/health/drugs/11086-non-steroidal-anti-inflammatory-medicines-nsaids. Accessed 17 Oct. 2022.
Jacques, Erica. Long-Term Use of NSAIDs for Chronic Pain and Potential Side Effects. Verywell Health, 3 Sept. 2022, https://www.verywellhealth.com/nsaids-for-chronic-pain-2564481#citation-3.
Huang ES, Strate LL, Ho WW, Lee SS, Chan AT. Long-term use of aspirin and the risk of gastrointestinal bleeding. Am J Med. 2011 May;124(5):426-33. doi: 10.1016/j.amjmed.2010.12.022. PMID: 21531232; PMCID: PMC3086018.
Fookes, C. Analgesic Combinations. Drugs.com, 29 May 2018, https://www.drugs.com/drug-class/analgesic-combinations.html.
Butalbital Compound. Drugs.com, https://www.drugs.com/mtm/butalbital-compound.html. Accessed 17 Oct. 2022.
Rapposelli, Dee. Complementary and Integrative Medicine in Migraine and Headache Management. Clinical Pain Advisor, 23 Aug. 2017, https://www.clinicalpainadvisor.com/migraine-headache/complementary-and-integrative-medicine-in-migraine-and-headache-management/#:~:text=Complementary%20and%20Integrative%20Medicine%20in%20Migraine%20and%20Headache,Applicability%20…%205%20Limitations%20…%206%20References%20.
Michael Ready, Duren. “Integrative Headache Management.” Integrative Pain Management, Oxford University Press, 2016, pp. 593–606. Crossref, doi:10.1093/med/9780199315246.003.0041.
Cathcart S, Petkov J, Winefield AH, Lushington K, Rolan P. Central mechanisms of stress-induced headache. Cephalalgia. 2010 Mar;30(3):285-95. doi: 10.1111/j.1468-2982.2009.01917.x. Epub 2010 Feb 1. PMID: 19614706.
Langevin, Helene, and Carolyn A. Bernstein. Acupuncture for Headache – Harvard Health. Harvard Health, 25 Jan. 2018, https://www.health.harvard.edu/blog/acupuncture-for-headache-2018012513146.
Martincik, Lukas and Seffinger, Michael A.. “Osteopathic Manipulative Therapy Efficacious for Patients With Chronic Migraines” Journal of Osteopathic Medicine, vol. 115, no. 10, 2015, pp. 628-628. https://doi.org/10.7556/jaoa.2015.127
Headaches and Chiropractic. ACA Today, https://www.acatoday.org/patients/headaches-and-chiropractic/#:~:text=Your%20doctor%20of%20chiropractic%20may%20do%20one%20or,ergonomics%20%28work%20postures%29%2C%20exercises%20and%20relaxation%20techniques.%20. Accessed 17 Oct. 2022.
Gach, Michael R. Acupressure for Headaches and Migraines. Acupressure Online Training, https://acupressure.com/articles/headaches-migraines/. Accessed 17 Oct. 2022.
Barmherzig R, Rajapakse T. Nutraceuticals and Behavioral Therapy for Headache. Curr Neurol Neurosci Rep. 2021 May 10;21(7):33. doi: 10.1007/s11910-021-01120-3. PMID: 33970348.
Rezaei Kelishadi M, Alavi Naeini A, Askari G, Khorvash F, Heidari Z. The efficacy of alpha-lipoic acid in improving oxidative, inflammatory, and mood status in women with episodic migraine in a randomised, double-blind, placebo-controlled clinical trial. Int J Clin Pract. 2021 Sep;75(9):e14455. doi: 10.1111/ijcp.14455. Epub 2021 Jul 5. PMID: 34105866.
Yablon LA, Mauskop A. Magnesium in headache. In: Vink R, Nechifor M, editors. Magnesium in the Central Nervous System [Internet]. Adelaide (AU): University of Adelaide Press; 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507271/.
Davenport. The Best Magnesium To Take For Headaches Is. IV Revival, 19 July 2021, https://ivrevival.com/the-best-magnesium-to-take-for-headaches/.
Gelfand AA, Goadsby PJ. The Role of Melatonin in the Treatment of Primary Headache Disorders. Headache. 2016 Sep;56(8):1257-66. doi: 10.1111/head.12862. Epub 2016 Jun 17. PMID: 27316772; PMCID: PMC5012937.
Brusie, Chaunie. Melatonin and Migraines: Does It Work? Healthline, 18 Mar. 2016, https://www.healthline.com/health/migraine/melatonin-and-migraines#What-Is-Melatonin?
How Does CGRP (Calcitonin Gene-Related Peptide) Cause Migraines? eMedicineHealth, https://www.emedicinehealth.com/how_does_cgrp_cause_migraine/article_em.htm. Accessed 17 Oct. 2022.
McCormick, Marya. Natural CGRP Receptor Antagonists. Minerals for Migraines, 3 Feb. 2017, https://mineralsformigraines.com/natural-cgrp-antagonists-migraine-relief/#Which_specific_plants_naturally_reduce_CGRP_levels.
Nayar D, Mahapatro M, Nayar P. Role of Yoga as an Adjunct in the Management of Migraine Headache-Current Status and Future Indications. Int J Yoga. 2022 Jan-Apr;15(1):12-18. doi: 10.4103/ijoy.ijoy_173_21. Epub 2022 Mar 21. PMID: 35444373; PMCID: PMC9015090.
Araujo, Laura. The 5 Beginner Yoga Poses That Everyone Needs to Know. 16 Feb. 2021, https://themapsinstitute.com/the-5-beginner-yoga-poses-that-everyone-needs-to-know/.
